
Overdiagnosis and over testing
The Medical Journal of Australia highlights the high carbon footprint of diagnostic testing. This was a study in secondary care, which has somewhat different issues from primary care, but the principle of acknowledging the carbon footprint of diagnostic testing remains pertinent. “The carbon footprint of common pathology tests was dominated by those of sample collection and phlebotomy. Although the carbon footprints were small, millions of tests are performed each year in Australia, and reducing unnecessary testing will be the most effective approach to reducing the carbon footprint of pathology. Together with the detrimental health and economic effects of unnecessary testing, our environmental findings should further motivate clinicians to test wisely.”
Overdiagnosis can contribute to patient harms and an increased carbon footprint of healthcare. Organisations such as the BMJ (Too Much Medicine Initiative) and the RCGP (Overdiagnosis group) have looked at tackling this issue, and joined together to produce the Better Medicine report.
Diagnosis can easily get lost between primary and secondary care. For instance a patient treated as having an asthma attack in A&E may or may not have asthma, and a clear process to ensure a sound diagnosis is important to ensure appropriate treatment.
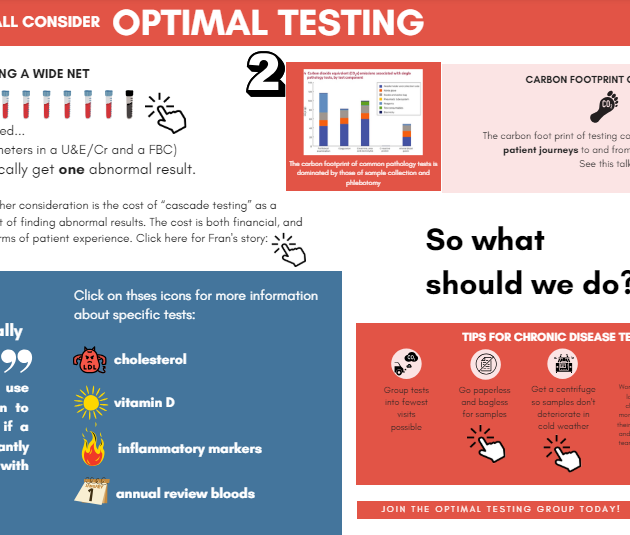
This infographic ‘OPTIMAL TESTING’ is a fantastic interactive resource taking you through various issues including screening, cholesterol checks and tests for fatigue.
Person centred medicine
Partnering with patients and supporting a focus on what matters to them can deliver health gains through patient empowerment and reduced harm and waste from unnecessary investigations, referrals and treatment. Useful resources on this subject can be found on Choosing Wisely, Realistic Medicine and from the Rethinking medicine.
You may also be interested in John Launer’s work on narrative based medicine, and for a holistic, de-medicalising approach to psychological distress, see the Power Threat Meaning framework hosted by the British Psychological Society.
Atul Gawande, in his book Being Mortal, gives tips about discussing decisions with patients, and “What matters to you” is becoming an increasingly important question in healthcare which can help us avoid overdiagnosis and overtreatment for some patients.
